From Targets to Treatments
How Miller School researchers advance drug discovery
By Josh Baxt
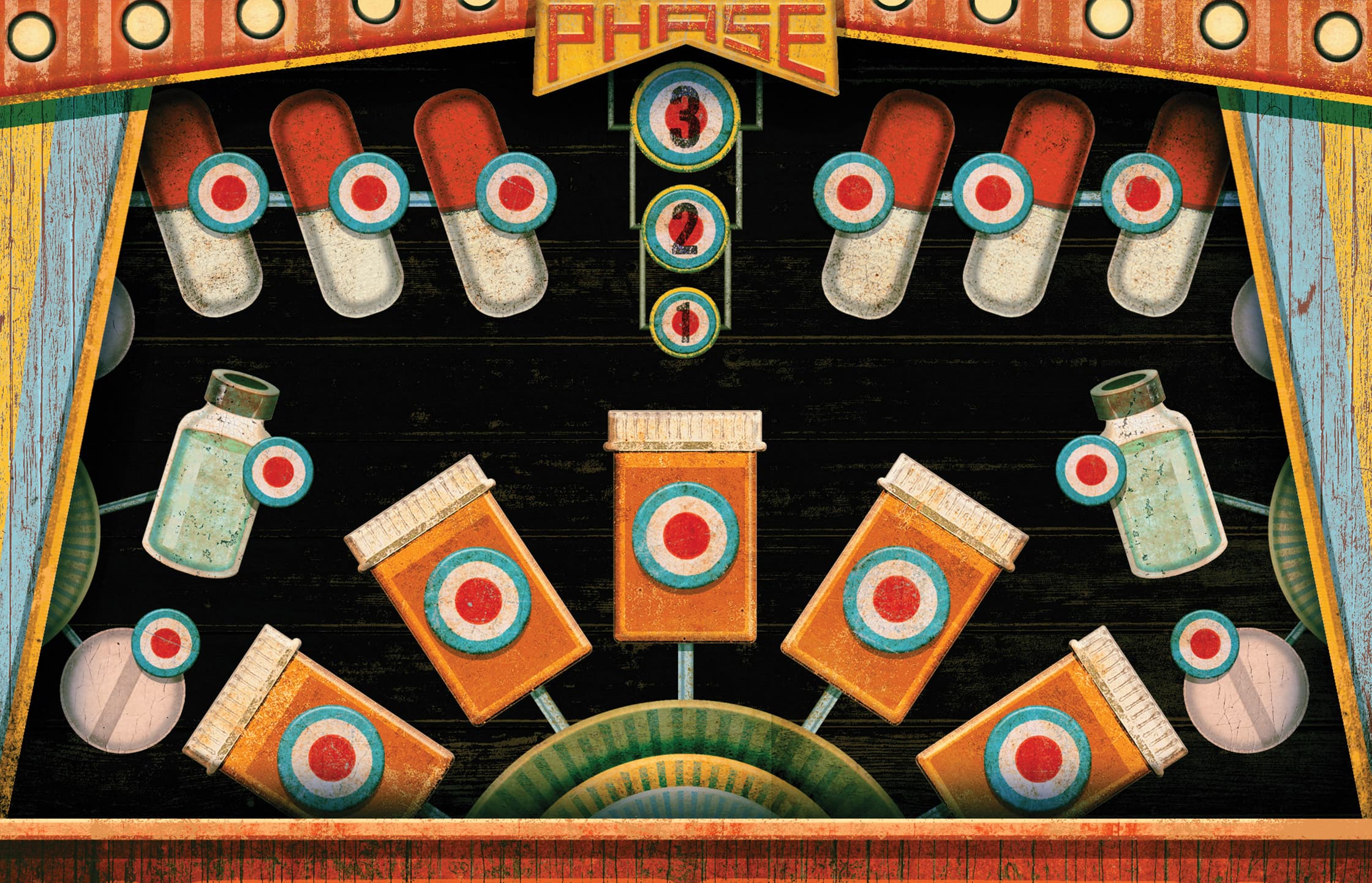
Illustration by Christian Northeast
F
undamental discovery research often begins with a series of questions. How does this cellular mechanism work? What are the signaling pathways that drive disease or preserve health? How can we manipulate these pathways for therapeutic benefit?
During this process, researchers often identify targets, usually proteins, that they can modulate to short-circuit disease signaling. An aberrant oncogene protein, for example, can be turned down to slow cancer progression.
Identifying a target is crucial to developing new drugs, but it’s just one step in a long, long journey. Researchers throughout the Miller School of Medicine are conducting a wide range of studies to identify potential targets and begin the early-phase drug discovery process that is so crucial to getting new medicines to patients.
The Center for Therapeutic Innovation seeks to unite scientists in their efforts to develop therapies for neurodegenerative conditions such as Alzheimer’s, cancer, rare genetic diseases, psychiatric disorders and others.
“Part of our role is to break down silos between disciplines,” said Claes Wahlestedt, M.D., Ph.D., who is CTI’s director and associate dean for therapeutic innovation, as well as a professor of psychiatry. “We work with people in many different departments, and we can act as connective tissue between researchers. If two people are doing complementary work, we can help bring them together.”
CTI is part of an emerging movement among academic researchers at the Miller School and elsewhere to play a larger role in drug discovery and accelerate efforts to bring medicines to patients. Here are five critical steps in making that happen.
1. Find a Target
Looking for drugs without a biological target would be like trying to fix a car without knowing exactly where the problem is. Scientists can spend years, even decades, investigating biological pathways to find potential targets for new medicines.
Researchers use a variety of tools, including cellular, animal and computational models, to understand these pathways and figure out how to manipulate them.
2. Develop the Right Molecule(s)
Once researchers have identified a potential therapeutic target, the next step is finding a molecule that will make it more or less active. Small molecule compounds are ideal because they can be administered orally and the chemistry is relatively straightforward.
Thirty years ago, finding therapeutic small molecules was almost entirely the domain of pharmaceutical companies. Today, academic researchers are taking a more active role, identifying compounds that might someday become vital medicines.
To find molecules that can modulate the target, scientists often use high-throughput screening platforms — intricate robotic devices that can test thousands of small molecules and determine which ones affect a particular target. Machine learning is being added to the mix, as well. While these in silico approaches cannot replace physical testing, they can identify subsets of molecules with greater potential, speeding up the process and reducing costs.
“We can’t do everything just by a computer,” Dr. Wahlestedt said, “but we can reduce the scope of a project. Instead of testing a hundred molecules, thanks to in silico work, we maybe reduce that to ten. Bringing somebody with computational expertise on board early can help a lot.”
Looking for drugs without a biological target would be like trying to fix a car without knowing exactly where the problem is.
3. Image Tiny Molecules
These screening campaigns often identify several promising molecules, or hits, which sets off a series of activities. Researchers use advanced imaging techniques, such as X-ray crystallography, to visualize where the small molecule binds to the protein, providing insights into how the reaction works and whether it shows promise as a possible drug.
These findings will also be important later in the process, as drug companies seek regulatory approval to begin clinical trials.
4. Optimize the Impact
At some point, the molecule is given to medicinal chemists and pharmacologists to optimize. Their goal is to refine the compound so that it binds better to the target protein — and only the target protein, to avoid potential side effects. Chemists also adjust the compound so it stays in the body longer and concentrates in areas where it can best fight disease.
“It’s a highly iterative process,” Dr. Wahlestedt said. “Chemists make the molecules, and pharmacologists or biologists test them. They’re trying to take the raw molecules and make them more drug-like so they can ultimately move forward into clinical trials.”
This too is a complex process, and it can take months to produce an optimal compound for further investigation.
5. Prepare for Human Trials
Once a compound is more or less finalized, researchers test it in cellular and animal models. This process can go on for some time, as scientists and regulators want to ensure the compound is safe before proceeding to human clinical trials.
“A drug can fail for two reasons: Either it’s not safe, or it lacks efficacy,” Dr. Wahlestedt said. “We’re hoping to show it has both.”
An equally important piece is identifying a biomarker for the drugs. A good biomarker can tell investigators whether the drug is working — crucial information during clinical trials. This is another tremendous strength for academic research. The same fundamental investigations that produced a therapeutic target in the first place can also identify good biomarkers. Industry often leans on its academic partners to find good biomarkers.
At some point during this process, the compound can be licensed to a company and proceed to phase 1 human trials to assess safety and determine the most appropriate dosage. If the drug is proven safe, it can proceed to phase 2, which begins to address efficacy in patients. If it passes that test, the drug proceeds to phase 3, a much larger study and typically the pivotal trial.
If the drug helps patients in phase 3, it usually goes on to receive approval from the U.S. Food and Drug Administration, European Medicines Agency and other regulatory bodies, and can then be used to treat patients worldwide.![]()


