A Volunteer Confronts the
Pandemic’s Epicenter
Melvin La, M.D. ’14, learned valuable lessons in New York City at the height of the COVID-19 crisis
By Priyanka Sinha
Photography by Winni Wintermeyer

I
n April, three days before Melvin La, M.D. ’14, arrived in New York City, there were more than 20,000 patients hospitalized with COVID-19 in area hospitals. The need was so overwhelming that Dr. La and 19 other University of California, San Francisco (UCSF) volunteers were beginning a one-month assignment providing urgently needed care for patients in the New York-Presbyterian (NYP) hospital system. The group arrived to find 2,500 inpatients with COVID-19, and the number was rising steadily as New York grappled with a major surge in infection rates.
“I looked out of the bus window on our way to Manhattan,” Dr. La said. “The streets were empty, businesses were closed, and it was eerily quiet. I remembered how alive and vibrant New York was before the pandemic. It was really heartbreaking.”
Volunteering in New York City was a homecoming of sorts for Dr. La, an anesthesiologist at UCSF, who completed his residency and fellowship at the very hospital his group was supporting.
“When I heard they were asking volunteers to go to New York, I couldn’t help but jump at the opportunity,” he said. “I knew a lot of the faculty there — some of my former co-residents are there now, and I knew many of the nurses as well. I really wanted to support them.”
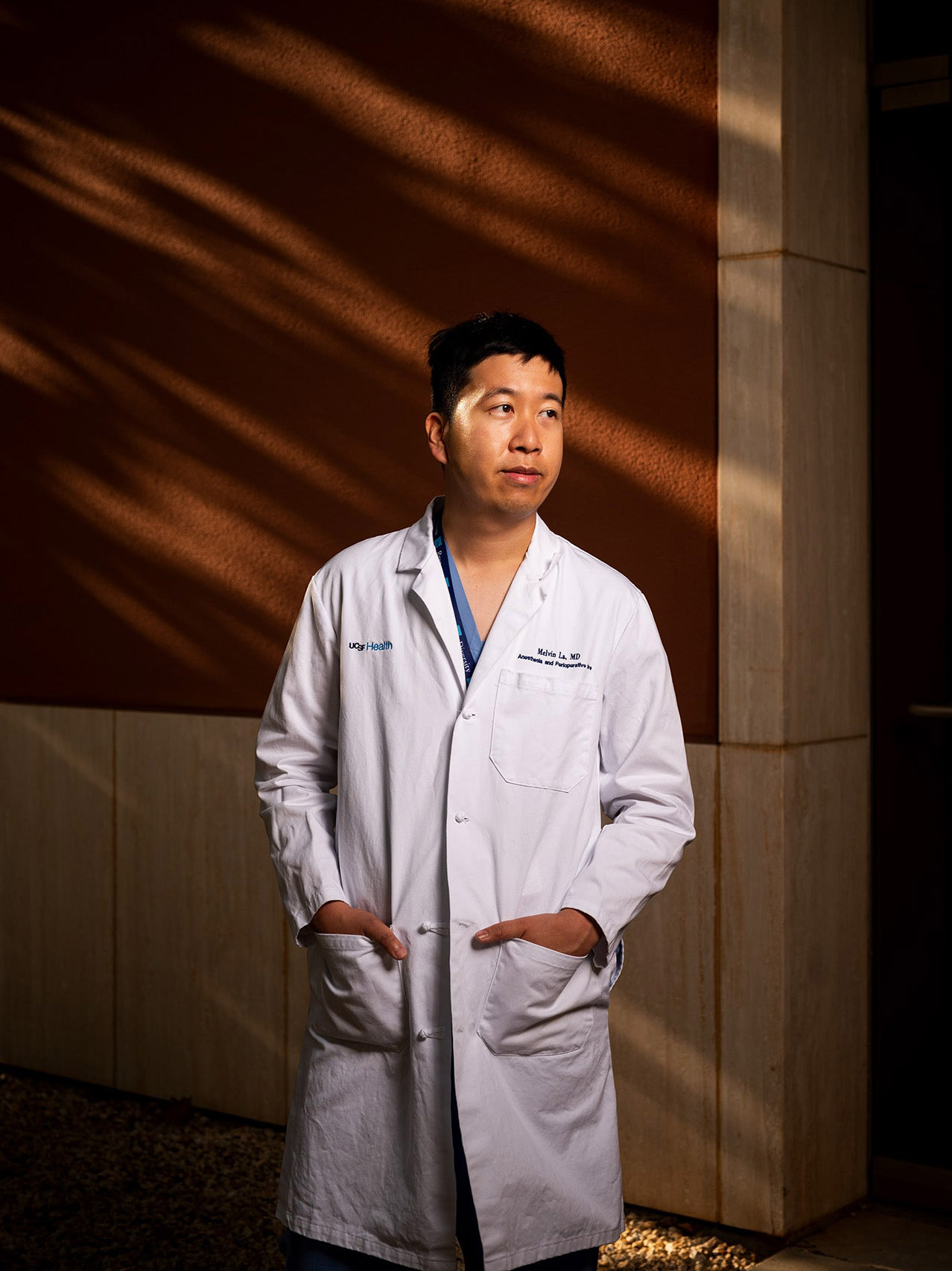
Melvin La, M.D. ’14
Required skills to battle a pandemic
The team of UCSF health care providers — 12 physicians and eight nurses — were selected from more than 50 physicians and 150 nurses who volunteered for the assignment. They all specialized in critical care, hospital medicine, and emergency medicine — key skills required in a pandemic setting.
Dr. La’s training prepared him for the urgent pace of the care he had to deliver. Two aspects of his expertise in particular reinforced his performance at NYP — his experience as an anesthesiologist and his training at the University of Miami Leonard M. Miller School of Medicine.
“We are airway experts,” Dr. La said. “We place breathing tubes and put people on ventilators — not just for routine surgery, but also for very sick patients. Thanks to the four to six months of ICU training in our residency, we’re kind of a versatile group.”
As the infection rates increased, so did the number of patients with severe respiratory problems activated by the immune system’s response to COVID-19. New York City hospitals had to act quickly and think creatively to meet the influx of very sick patients. NYP repurposed operating rooms and anesthesia machines for patients who needed ventilators.
“We had 40 patients in operating rooms on machines, on top of the 100 to 150 patients in other locations on ventilators,” Dr. La said. “They needed people who were familiar with operating those anesthesia machines, which had been repurposed from their original use to ventilate patients.”
Dr. La credits his training at the Miller School for giving him the mindset and talent required to serve during the crisis.
“For as long as I can remember, I wanted to use science to help others,” he said. “As a student at the Miller School, I had all sorts of opportunities to be involved with community service and really make a difference in people’s lives. Those experiences are with me every day.”
Patients suffered without their loved ones
Service during a pandemic had its poignant moments for Dr. La, such as treating patients who had no family members or loved ones by their bedside.
“It was the most heartbreaking thing to see these patients suffer by themselves, and to see many of them even pass away all alone without their families close by,” he said.
One COVID-19 patient on a ventilator, in a drug-induced coma at NYP, was no more than 40 years old. Every morning, Dr. La passed his bedside and saw a photo of the man in good health with his wife and children.
“Below the photo was a note to the ICU team from his wife describing the patient and who he was — an active family man — and asking us to take care of him as much as possible,” Dr. La recalls. “It was tough, but inspiring as well, and kept us focused on doing our best to care for those patients.”
New York City, stronger together
While the pandemic brought on untold suffering for many families and strained the health care system beyond its capacity at times, it also brought a community together. New York City dealt with the surge methodically and with a sense of collective pride for health care workers on the front lines.
“It was truly amazing to see how the city came together in this time of crisis,” Dr. La said. “Even though the streets were empty and businesses closed, the restaurants and community at large were sending food to the hospitals. We never really went hungry the entire time.”
Dr. La was also deeply moved by the cheering that took place every evening. As health care workers would start or complete their 12-hour shifts, New Yorkers near the hospital would show their appreciation by honking their horns or clapping and banging pots and pans from their windows.
“Despite how very isolated one could feel, you knew you were part of something bigger in New York, helping out this community,” he said.
Staying safe and the tenacity of COVID-19
Dealing with a highly infectious virus gave the UCSF team a greater appreciation for the kind of protection needed to stay safe. They followed rigorous safety guidelines, with strict adherence to hand hygiene and wearing personal protective equipment when treating patients.
“Even though we spent four weeks in what was the epicenter of the pandemic, directly treating COVID-19 patients, none of us got sick,” Dr. La said.
Dr. La also came away with a greater sense of appreciation for the tenacity of COVID-19. He found out how difficult it was to get patients back to their baseline functions. Many patients were on ventilators in the ICU for weeks, which is unique compared with standard respiratory illnesses.
“Once the initial phase of an illness passes, patients are usually very quick to come off ventilators,” Dr. La said. “By contrast, COVID-19 patients stay intubated for weeks on end. It’s incredible to see how persistent this virus is.”
While the pandemic has affected every part of society, regulating every daily activity, Dr. La’s time in New York taught him not to be tricked into a false sense of security. The persistence of COVID-19 and its complex impact on the human body can be devastating.
“We must steel our resolve even further for the months to come and help each other stay safe and optimistic,” Dr. La said. “From what I’ve seen in New York City, we can get through anything. It takes the strength of a community working together to eradicate this virus.”![]()
Visit the Medical Alumni Association website for alumni news, event updates, and ways to stay connected.


