Is This the End of HIV?

Not yet, but Miller School researchers and clinicians are part of a decades-long effort that is closing in on a cure
By Josh Baxt
Illustrations by James Taylor
 n the early 1980s, Savita Pahwa, M.D., was director of immunology at North Shore University Hospital in Long Island, New York, when an unnamed disease began killing children. She thinks about them often. “I remember all the beautiful children,” she said. “I had such close relationships with them.”
n the early 1980s, Savita Pahwa, M.D., was director of immunology at North Shore University Hospital in Long Island, New York, when an unnamed disease began killing children. She thinks about them often. “I remember all the beautiful children,” she said. “I had such close relationships with them.”
Dr. Pahwa wrote the first definitive paper about how a virus affected children’s immune systems. The disease was so new, the term human immunodeficiency virus, or HIV, didn’t yet exist. In the study, she called it human T-cell lymphotropic virus (HTLV-III).
At the University of Miami, physicians like Gwendolyn Scott, M.D., now professor emeritus of pediatrics, were also seeing how this new disease was affecting children.
“In the early years of the HIV epidemic, there was a lot of fear and stigma since we did not understand what caused the disease or how it was transmitted, and there were no specific treatments,” said Dr. Scott, an infectious disease specialist. “The mortality rate was incredibly high, and families were frequently alone in coping with it. Many infected infants suffered an early death.”
Around the same time, Margaret Fischl, M.D. ’76, professor of medicine and director of the AIDS Clinical Research Unit, and colleagues were treating adults with AIDS. Contrary to the “gay plague” epithet, they found the virus was affecting heterosexuals, particularly in the Haitian community. Initially, the U.S. Centers for Disease Control and Prevention rejected these findings, thinking the UM team was seeing a different disease, but eventually the agency came around.
HIV was finally identified in 1983, and that led to clinical progress. UM clinicians were among the first to provide antibody tests and culture the retrovirus to diagnose patients. Forty years later, physician-researchers at the Miller School are still on the cutting edge of HIV/AIDS research, working to understand the disease from many different angles, providing treatments and support for those living with the virus, and imagining a near future in which new infections drop by 90%.
“We’ve made amazing progress,” said Dr. Pahwa, “but the virus remains a master at evading the immune system. We know what it’s doing, we just haven’t been able to defeat it yet.”
A Series of Breakthroughs
 n the beginning, we were involved in describing the epidemic — how it was transmitted, who was getting infected, the symptoms, the complications, the processes — and that put us immediately into the forefront of treatment,” Dr. Fischl said. “We began treating not only the complications –— pneumonias, serious brain infections, tumors — but we also began to realize that you could actually get at this virus. The first HIV drug ever tested was tested at the Miami site.”
n the beginning, we were involved in describing the epidemic — how it was transmitted, who was getting infected, the symptoms, the complications, the processes — and that put us immediately into the forefront of treatment,” Dr. Fischl said. “We began treating not only the complications –— pneumonias, serious brain infections, tumors — but we also began to realize that you could actually get at this virus. The first HIV drug ever tested was tested at the Miami site.”
Dr. Fischl and others at the medical school played a critical role in recognizing the value of AZT, the first FDA-approved drug to treat AIDS. Equally important, the drug tamped down virus transmission from mother to baby.
“One of our big triumphs was giving AZT to pregnant women and then to their babies for six weeks after delivery,” Dr. Scott said. “This decreased the number of perinatal transmission cases by two-thirds. It was a total miracle. They stopped the trial early because it was such a success. That was a real turning point for preventing HIV in children.”
Another breakthrough came in 1996, when highly active anti-retroviral therapy, or ART, transformed HIV from a deadly disease to a chronic one. People went from dying in a matter of months or a couple of years to living nearly normal lifespans.
There are now 35 FDA-approved anti-retroviral drugs. Children with HIV are surviving and even having children of their own. By bringing the viral load to undetectable levels, ART and other treatments have virtually eliminated transmission from pregnant women to their babies and between sexual partners.
A Tricky Virus
ART controls the virus but never fully destroys it. HIV knows how to play hide and seek with the immune system. Under treatment, the virus hibernates. If a patient stops taking their medications, it wakes up.
“HIV establishes long-lived reservoirs that persist indefinitely, even when people are on effective therapy,” Dr. Pahwa said. “That’s because the viral DNA integrates into the host genes in CD4 T cells. When they are in a resting state, there is no way to tell if it’s an infected cell or a normal one. The immune system just can’t see it.”
CD4 memory T cells are perhaps the most essential immune system components. They are also the main cells that HIV infects. CD4 T cells help B cells make antibodies, and CD8 (cytotoxic) T cells attack infected cells.
“They’re called memory T cells because they live a long time and rarely forget a pathogen,” said Mario Stevenson, Ph.D., professor of medicine and director of the HIV and Emerging Infectious Diseases Institute (HEIDI) at the University of Miami.
When the immune system knocks out a measles virus it first encountered during a tearful pediatric visit decades before, it’s CD4 T cells taking command. Active HIV destroys CD4 cells, eliminating that leadership.
Researchers have developed a strategy called “shock and kill” to root out the virus. The idea is simple: Shock HIV out of hibernation and destroy it. But that is easier said than done. HIV is built to mutate, and many of these mutations render the virus inert. This can make it difficult to determine which infected CD4 cells are dangerous.
But the greatest challenge may be in detecting where dormant HIV-positive T cells live. While it’s relatively easy to find infected immune cells in blood, there are other, more secretive hiding places. The majority of hidden HIV lives in immune cells, including myeloid cells, which patrol various tissues to fight off disease.
Even collecting myeloid cells for study is challenging. As a result, scientists don’t really know where the virus may be hiding. The liver? Lungs? Brain? Dr. Stevenson’s lab has developed an indirect way to find where viral particles originate: He simply asks them.
“We’ve found that the viral particles have these tiny molecular address tags,” Dr. Stevenson said. “If an individual discontinues therapy and the virus rebounds, we can collect it and look for its address label. We’ve developed assays that look at the composition of the virus that give us clues to what kinds of cell it originated in — T or myeloid — and where that cell was located.”
Understanding HIV’s secret life is a necessary early step toward shocking those hibernating cells awake and destroying them with ART or other therapies. But even that is tricky. Shocking T cells can generate a runaway immune response. Another strategy may offer a more nuanced approach.
“A large number of labs are looking at creative ways to eliminate these hidey-holes using gene therapy, immune modulators and antibodies,” Dr. Stevenson said. “They’re not trying to shock and kill but rather shock and lock. They’re not removing HIV, just making it inert.”
DESTROYING A VIRUS THAT HIDES✱
DESTROYING A VIRUS THAT HIDES✱

Listen to Dr. Mario Stevenson’s podcast discussion with Dean Henri Ford about how HIV remains dormant in cells
Community Outreach Meets Lab Science
 With Miami the epicenter of the United States’ HIV/AIDS epidemic, accounting for one-third of new HIV diagnoses in Florida, Miller School faculty are actively working to help vulnerable, HIV-infected populations. One effort is the IDEA Exchange, Florida’s first legal syringe exchange program, which was co-founded by Hansel Tookes, M.D. ’14, M.P.H. ’09, associate professor of medicine (see page 22).
With Miami the epicenter of the United States’ HIV/AIDS epidemic, accounting for one-third of new HIV diagnoses in Florida, Miller School faculty are actively working to help vulnerable, HIV-infected populations. One effort is the IDEA Exchange, Florida’s first legal syringe exchange program, which was co-founded by Hansel Tookes, M.D. ’14, M.P.H. ’09, associate professor of medicine (see page 22).
The Center for HIV and Research on Mental Health, or CHARM, directed by Professor of Psychology Steven Safren, Ph.D., focuses on helping people with HIV who may also have mental health and/or substance abuse issues. The goal is to help modify behaviors to improve their health and prevent transmission.
“We support investigators who conduct research related to HIV and mental health,” Dr. Safren said. “We are particularly interested in research that’s going to inform policy and practice and help the community, as well as getting HIV transmission to zero.”
Dr. Safren noted that pre-exposure prophylaxis (PrEP), a medication that helps prevent HIV transmission, can be incredibly effective. Unfortunately, PrEP is not being used consistently in many underserved communities.
“PrEP really helps with HIV prevention,” he said. “However, many populations don’t have access to it, and we want to address that disparity.”
Dr. Pahwa established Miami Center for AIDS Research, or CFAR, in 2007. One of 19 such centers around the country, the program spurred HIV research in South Florida. Dozens of scientists are channeling nearly $30 million in grants each year to study and control HIV. In addition, a new generation of researchers is benefiting from pilot grants and other funding. (CFAR is part of an interconnected network of UM research groups, including HEIDI, the Clinical and Translational Science Institute, and Sylvester Comprehensive Cancer Center.)
Drs. Tookes and Stevenson recently received a $3.1 million grant from the National Institute on Drug Abuse to determine how methamphetamine use affects the HIV virus in men who have sex with men. Called ARES, the study follows participants for six months, testing their viral loads, immune responses, psychiatric status and other markers to better understand how methamphetamine influences HIV progression. While the primary focus is community support, the ARES study will also give researchers in the Stevenson lab new opportunities to interrogate how methamphetamine use wakes up HIV-infected cells.
“One of our suspicions is that substances like meth might trigger the virus to be more alert — to be less in the slumber mode and more in the active mode,” Dr. Stevenson said. “It’s a double-edged sword. On the one side, active HIV is not good for the individual’s health. However, if the virus is more alert, it might be more visible to the immune system and antiretroviral agents. These are the mechanisms we want to understand.”
CHARM is a National Institutes for Mental Health-funded AIDS Research Center and also relies on philanthropy to support numerous research projects. As with CFAR, many studies are conducted by junior investigators. CHARM support helps jump-start their research and get external funding to expand their work.
One program, called CHANGE (Culturally focused HIV Advancements through the Next Generation for Equity), was launched in 2021 to train the next generation of HIV behavioral scientists. Led by Sannisha Dale, Ph.D., associate professor of psychology, and Daniel Feaster, Ph.D. ’00, and Viviana Horigian, M.D., M.H.A., both professors of public health sciences, the program trains predoctoral and postdoctoral fellows to pursue high-impact research and reduce mental health inequities in Black, Latino and LGBTQ communities.
“Science is failing minoritized populations in the U.S.,” Dr. Horigian said. “Adequate pipelines of training for the professional development of minoritized scientists are scarce, and research is not focusing effectively on the disparities affecting these populations. CHANGE is a result of our institutional commitment to combating racial injustice.”
Candice Sternberg, M.D., assistant professor medicine in the Division of Infectious Diseases, is working to improve HIV care and PrEP access in Miami’s Haitian community. Dr. Sternberg wants to partner with churches, television and radio stations and other groups to raise awareness about PrEP. As a Haitian American, she often uses her personal relationship with the community to help cement change.
“I have been able to do a lot of research there because I’m a member of the community and can speak to people in their native language,” Dr. Sternberg said. “I think people are more receptive to having someone from within the community talk to them about these issues and guide them to better care.”
Countering Risk with Education
Longtime HIV fighter Sonjia Kenya, Ed.D., M.S., M.A., professor of medicine and public health sciences, is known for her unconventional approaches to reducing the incidence of HIV/AIDS in underserved neighborhoods. She explains how one of them — CHAMP (Community-based HIV Awareness & Testing for Minority Populations) — creates bonds with residents at risk.
By Joey Garcia
Illustration by James Taylor

Why is Miami-Dade — and especially Liberty City — the epicenter for new HIV infections in the United States?
Lack of access to culturally informed HIV education and to health care are the driving factors for excess HIV infections in Liberty City. There is no accessible, comprehensive HIV care in Liberty City, and to my knowledge, CHAMP is the only street-based team composed of culturally representative Black community health workers focused on reducing HIV in this community. While other health providers rotate in and out of Liberty City, most employ non-Black staff, which can function as a barrier to care since the team members don’t look like or speak like the population they’re attempting to serve.
Does knowing the “why” help combat HIV through better education, treatments or other initiatives?
Yes, knowing why people don’t practice protective sexual behaviors does help our team develop behavior-specific interventions. For example, CHAMP hosted a workshop titled “Are You the Side Chick?” in response to Liberty City residents telling us that numerous women were having sexual relations with the same man who was HIV positive. While the women knew they were in a non-monogamous relationship, they did not understand their HIV risk. As a result, the workshop we hosted prompted women to consider their sexual relationships within the context of HIV risk. Once they understood that non-monogamy was associated with increased HIV risk, they could make informed decisions about whether they wanted to be the “side chick.”
How do you reach out to the community?
We have numerous community engagement events several times per month and a robust social media presence in which community members can send us direct messages to obtain on-call services. At least once per month, we host a health awareness event addressing issues the community has brought to our attention. It’s not always about HIV — it’s about building healthier communities and trust with residents so they feel comfortable reaching out to us for assistance with HIV or any other health concern. Outreach is shared among the 12 team members, and specific community health workers conduct outreach at different times of day and night to ensure all residents have access. We have four full-time testers, and the last full year of HIV testing data showed CHAMP tested about 1,000 individuals annually, which breaks down to about 85 people per month. The rest of the team is focused on linking HIV-positive people to care and supporting them with medication adherence in order to achieve optimal HIV outcomes.
What are the demographic statistics?
Ninety-five percent of our participants are Black, and the remaining are majority Latin/Hispanic. We test people ages 13-82, and the median age of participants is 43 years old. With regard to gender, our sample is equally split between males and females.
Numbers are rising again. Is that because there was less testing during the pandemic? Or are there other factors?
The pandemic disrupted HIV care, and the World Health Organization has estimated at least 500,000 excess deaths from HIV would result from this disruption of services during the pandemic. Other contributing factors include reduced efforts from health care providers focused on HIV. With the onset of COVID-19, HIV funding decreased substantially, and HIV took a back seat in infectious disease control. Ironically, the same people who suffer from the worst HIV outcomes also suffer from the worst COVID-19 outcomes, and we did secure funding to address COVID-19 in our communities of focus.
HIV is a preventable disease. Why do people indulge in risky behaviors?
While HIV is preventable, many people of low socioeconomic status do not have easy access to condoms or PrEP, and they don’t know that these resources can be obtained free of charge at public health clinics. While much information is available, it is rarely conveyed in a culturally tailored manner to reach the populations that need it most. If condoms, PrEP and culturally representative community health workers were available at no cost on every corner of low-income neighborhoods, HIV disparities would not be so prevalent in these communities.
What new programs are you planning?
I plan to expand our street-based community health worker teams to other geographic locations where Black people suffer poor HIV outcomes. As current HIV therapies are underutilized by Black people and the cure for HIV will soon become a reality, it’s critically important to ensure trustworthy HIV-prevention efforts are in place to ensure Black people benefit equitably from these advances. My hope is these efforts help eliminate HIV disparities in Blacks and contribute to policy development enabling vulnerable Black patients to receive free support from culturally representative community health workers.
What do you think it will really take to end HIV?
Scientifically, we’re almost there, and I am confident a cure will be available within the next decade. However, to eliminate HIV among the most vulnerable populations, it is critically important for historically marginalized patients to know about the treatment and to trust HIV providers and the health care system so they feel confident in taking the treatment.
Living with HIV
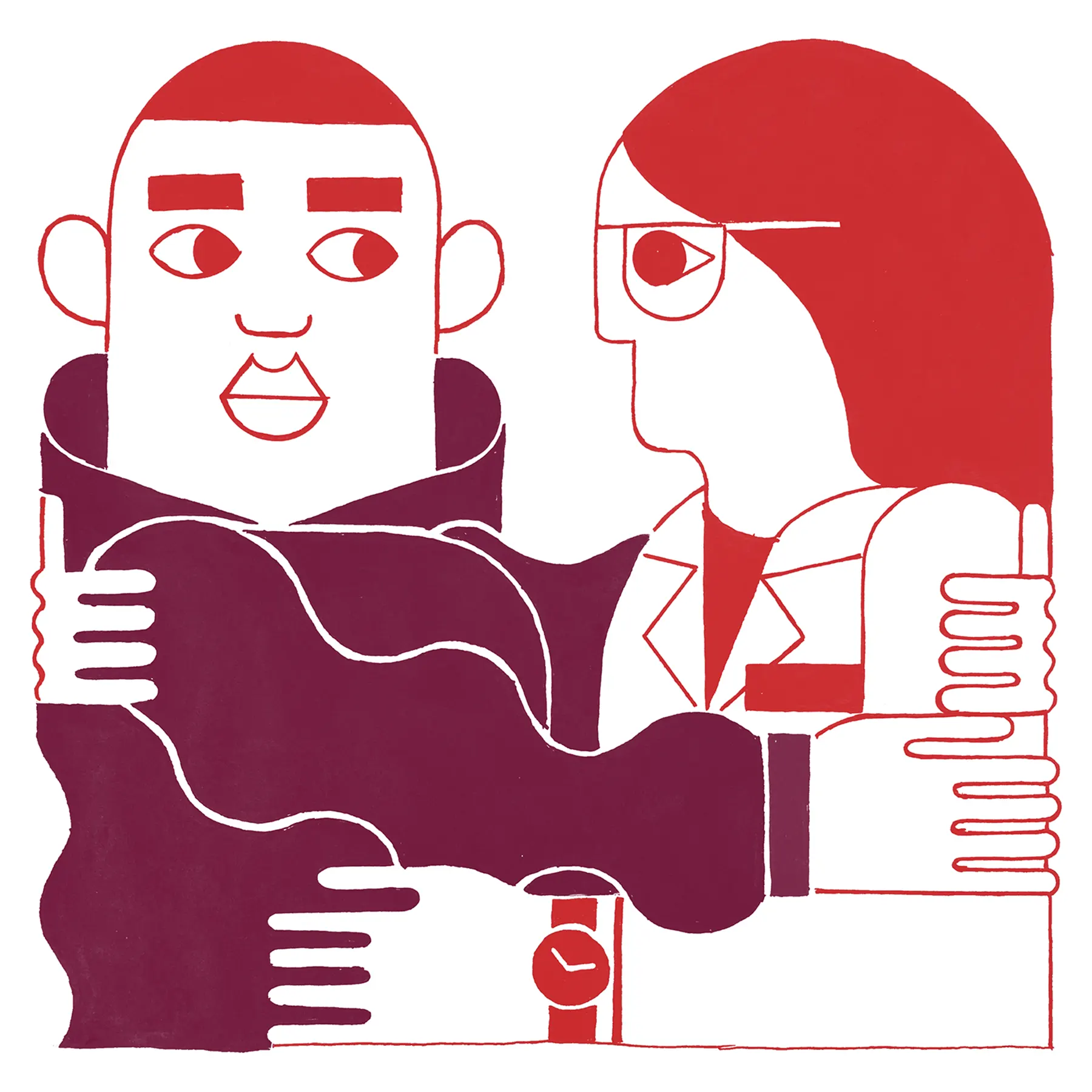
 ven 40 years after the virus was identified, researchers are still trying to understand how HIV operates. Maria Alcaide, M.D., a professor of medicine who studies infectious diseases and is director of clinical research at the Miller School, and Deborah Jones Weiss, Ph.D., professor of psychiatry and behavioral sciences and co-director of CHARM, are collaborating on several interdisciplinary studies to improve quality of life for people living with HIV.
ven 40 years after the virus was identified, researchers are still trying to understand how HIV operates. Maria Alcaide, M.D., a professor of medicine who studies infectious diseases and is director of clinical research at the Miller School, and Deborah Jones Weiss, Ph.D., professor of psychiatry and behavioral sciences and co-director of CHARM, are collaborating on several interdisciplinary studies to improve quality of life for people living with HIV.
Dr. Alcaide approaches these studies from the clinical side, while Dr. Weiss focuses on behavioral medicine. “My interest is not the clinical or lab part but the people part,” said Dr. Weiss. “Because HIV is complex, there are so many different behavioral issues around protecting yourself, taking care of yourself and not spreading the disease.”
Under their leadership, the Miller School is a major site for the MACS/WIHS Combined Cohort Study, a decades-long effort to investigate aging in people with HIV. “Most people living with HIV in the U.S. are over 50,” Dr. Alcaide said. “Although we have good ways to treat HIV and they can live long and healthy for many years, they are aging faster.”
The research team has received a seven-year, $14 million NIH grant to study these issues. Identifying the factors that precipitate accelerated aging could help many people live longer, including those who are not infected.
Drs. Alcaide and Weiss have also received a five-year, $15 million grant to study younger women infected with HIV, investigating the virus’s impact on reproductive, mental and oral health. Oral health is a particularly important component. In another study, called CROWN, the team is studying the confluence of oral and mental health and the impact on overall well-being.
“When people have inflammation, it’s not just in the mouth,” said Dr. Alcaide. “Inflammation can be systemic, and that has been associated with markers for other diseases, including heart disease. In addition, people with poor oral health may not eat well and have poor nutrition. It may also affect their sleep, which has an enormous impact on their quality of life.”
One of the major concerns is making sure people get the care they need. HIV patients must take their medications consistently for decades to remain healthy, and compliance can be an issue. However, Drs. Weiss and Alcaide are working to keep people in treatment.
“We’ve started using a strategy called motivational interviewing to help physicians reengage people in care,” Dr. Weiss said. “This has been quite effective, because it’s the people who stop taking their medication who are more likely to die from the virus.”
Separately, cardiologist Claudia Martinez, M.D., professor of medicine, is focusing on the dangerous triumvirate of HIV, inflammation and heart disease. She is leading a four-year, multi-center study, funded by a $2.8 million grant from the National Heart, Lung, and Blood Institute, to investigate elevated cardiovascular risk in HIV patients; some patients have had fatal heart attacks in their 20s or 30s. The study will examine factors on the surface of body cells — a type of lipids, called eicosanoids, that mediate inflammation — that react when HIV or certain other viruses invade them.
“The hope is to identify targets that will help decrease inflammation in its tracks, reducing cardiovascular disease, the No. 1 cause of death in this population today,” Dr. Martinez said. “No one has looked into this before, in part because the ability to measure the eicosanoid activity is a recent advance.”
Roger McIntosh, Ph.D., associate professor of psychology, is exploring how people living with HIV and other inflammatory conditions, such as cardiovascular disease, are affected by environmental factors.
“If people are immunocompromised but are also exposed to a lot of stress, that really breaks down their resilience,” Dr. McIntosh said. “My work is really looking at what type of psychosocial factors accelerate aging and other processes and what factors can instill resilience.”
He and his colleagues have been using functional magnetic resonance imaging and other techniques to look at how stress impacts the brain. Unfortunately, it’s difficult to re-create the kinds of stressors people experience in real life in the lab. To overcome that, Dr. McIntosh recently received a grant to bring the lab into communities, using an approach called ecological momentary assessments (EMA). The team is now collecting data in people’s day-to-day environments to better understand how stress may be impacting their biology.
“With psychological metrics, for example, if someone comes into the lab, we can ask them how stressed they’ve been over the past two weeks,” he said. “But there could have been a lot of high stress and a lot of low stress. We’re really just looking at averages. With EMA, we can look at moment-to-moment changes alongside biomarkers for inflammatory and cardiovascular risk.”
Harm Reduction Takes Center Stage
The IDEA Exchange sets the Florida standard for safety
By Joey Garcia
Illustration by James Taylor
While research is underway to cure HIV/AIDS, action is needed for those currently at risk for or living with HIV. Hansel Tookes, M.D. ’14, M.P.H. ’09, associate professor of medicine at the Miller School, recognized this need as a medical student. The proximity of the campus to at-risk populations inspired him to create the IDEA Exchange, the first legal harm-reduction program in Florida.
Since 2016, the IDEA (Infectious Disease Elimination Act) Exchange has been operating as a fixed clinic at the Miller School, with a mobile unit formed in 2017 to serve Greater Miami-Dade County. The facility, located near Overtown, offers safe injection packs, wound care, medications for addiction, naloxone (medication used for drug overdose reversals) and comprehensive care for HIV and hepatitis C.
“Our program meets people where they are both mentally and physically,” Dr. Tookes said. “Our primary demographic consists of 74% people who use opioids and 17% using both opioids and cocaine. We see people from all walks of life come to our program, as there is no judgment here, and substance use disorder does not discriminate. The goal is for our services to be used and to eliminate the spread of HIV.”
More than 2,000 people are enrolled the IDEA Exchange, with clean needles being the most requested service. Without the program, many of the people who use drugs in the area wouldn’t be in care or know of their status, further contributing to the rising HIV/AIDS rates in Miami-Dade County. The diversity of the program reflects that of the county, with the majority of participants from racial and ethnic minority groups.
Dr. Tookes noted a decline in overdose deaths with the distribution of naloxone, and 78% of participants with HIV are aware of their status, in care at IDEA, and are virally suppressed, “which is the highest I have seen reported in the literature among people who inject drugs,” he said. The IDEA Exchange has been an influential public health institution in the county and serves as the model exchange program statewide.
“I never could have predicted that this program would become so much more than a place where people can access injection equipment,” Dr. Tookes said. “Now the IDEA Exchange is this innovation lab that has impacted the state policy with the statewide expansion, medical education under our harm-reduction-focused substance use curriculum in NextGenMD and beyond.”
An HIV History
1981
– First report of mysterious new illness
1983
– Discovery of the AIDS virus
1985
– FDA approves serologic test for HIV diagnosis
1986
– Cause of AIDS virus given HIV name
1987
– FDA approval of AZT
1988
– CFAR program launched
1994
– Two-drug cocktail approved
1995
– Test for plasma virus load approved
1996
– Three-drug ART cocktail approved; death rate from HIV begins to fall in U.S.
2007
– Miami CFAR launched; FDA approval of integrase inhibitor (Raltegravir)
2012
– FDA approval of Truvada for PrEP
2016
– Survival gap narrowed to 9 years
2022
– First reports of tentative HIV cures
2030
– Federal target date to reduce HIV in U.S. by 90%
Long-term Care for HIV Patients
A positive diagnosis triggers opportunities for a healthy life
By Joey Garcia
Illustration by James Taylor
Many programs focus on the prevention of HIV/AIDS, but what happens to people who already are infected? The answer is long-term care, said infectious disease clinician Michael A. Kolber, M.D. ’83, Ph.D., professor of medicine; vice chair of compliance, quality and care transformation; and director of the Comprehensive AIDS Program, or CAPS.
CAPS provides HIV treatment to more than 3,000 patients in Miami-Dade County. People who test positive for HIV are referred to the adult HIV clinics, where they are registered and provided with care. As the majority of patients seen in the clinics are struggling economically, the program is foundational in supporting the services that provide care to these individuals, including specialty care, mental health, case managers and even hospital-based care.
“Our program supports the already established services throughout the medical campus,” Dr. Kolber said. “With the help of the Ryan White Care Act, HIV treatment is available at little to no cost to those needing treatment while we provide them with cutting-edge opportunities to continue living healthy lives despite their diagnosis.”
The clinic and CAPS serve a disadvantaged, predominantly minority population that is roughly 50% Black/African American, 10% Haitian, 30% Hispanic and 20% White individuals. The program’s reach extends past the primary care clinics in its support of patients with psychiatric and neurocognitive dysfunction, HIV patients who attend the IDEA Exchange needle-exchange program (story, page TK), patients with gynecologic issues, test-and-treat initiatives to ensure rapid access into care, and any specialty/subspecialty for problems related to their HIV disease. CAPS staff, under aegis of the AIDS Education and Training Center, have educated the South Florida provider community about issues related to ending the HIV epidemic, with attention to provision of PrEP (story, page TK), testing and issues pertinent to the care and understanding of the needs for people living with HIV.
“Everything we do is for the community,” Dr. Kolber said. “We all try to work together to integrate care opportunities for patients who may not have had them before. As our work is connected to the researchers and clinicians on campus, we don’t have silos. We try to integrate ways for patients to benefit from research, other programs and educational opportunities.”
The Possibility of a Cure
 IV is incurable, but there are tantalizing hints that more effective treatments are on the way. A tiny group of four patients — one of whom was in a study Dr. Pahwa worked on — have successfully gone off ART. All four had HIV and leukemia and received stem cell transplants with cells lacking the CCR5 protein, which helps HIV enter cells. While this approach cannot be scaled for the larger HIV population, it has generated great interest as researchers pursue gene and other therapies targeting CCR5.
IV is incurable, but there are tantalizing hints that more effective treatments are on the way. A tiny group of four patients — one of whom was in a study Dr. Pahwa worked on — have successfully gone off ART. All four had HIV and leukemia and received stem cell transplants with cells lacking the CCR5 protein, which helps HIV enter cells. While this approach cannot be scaled for the larger HIV population, it has generated great interest as researchers pursue gene and other therapies targeting CCR5.
Ronald Desrosiers, M.D., Ph.D., professor of pathology, has a long history of working on HIV. He was the first to identify SIV, the primate version of the virus, and has had preclinical success with a potential HIV vaccine. The treatment is built around a rare species of broadly neutralizing antibodies. While patients generate antibodies against their own HIV strains, the mutating virus eventually escapes this response. However, some people make broadly neutralizing molecules that attack most HIV strains.
The Desrosiers lab has combined genes from these antibodies with a virus that delivers them to muscle tissue, where they essentially become antibody factories. Early-stage research in primates has shown this strategy can be quite effective.
“It has been seven years since we did the intramuscular injection in one of our models,” Dr. Desrosiers said. “Approximately 2% of all circulating antibodies today are coming from the gene we put into that muscle seven years ago. These potent, broadly neutralizing antibodies could prevent infection in high-risk individuals or treat those who are already infected.”
While this one-shot-and-you’re-done approach has shown genuine promise, there’s still a complication: The antibodies in the therapy are so rare and exotic that the body often treats them as intruders. As a result, these therapeutic antibodies are neutralized by the body’s own antibodies, negating their impact.
“Most of the work in my lab over the past few years has been focused on finding simple, readily applicable ways to create antigen-specific tolerance,” Dr. Desrosiers said. “We need to teach the body that these antibodies are not foreign.”
A Positive Outlook
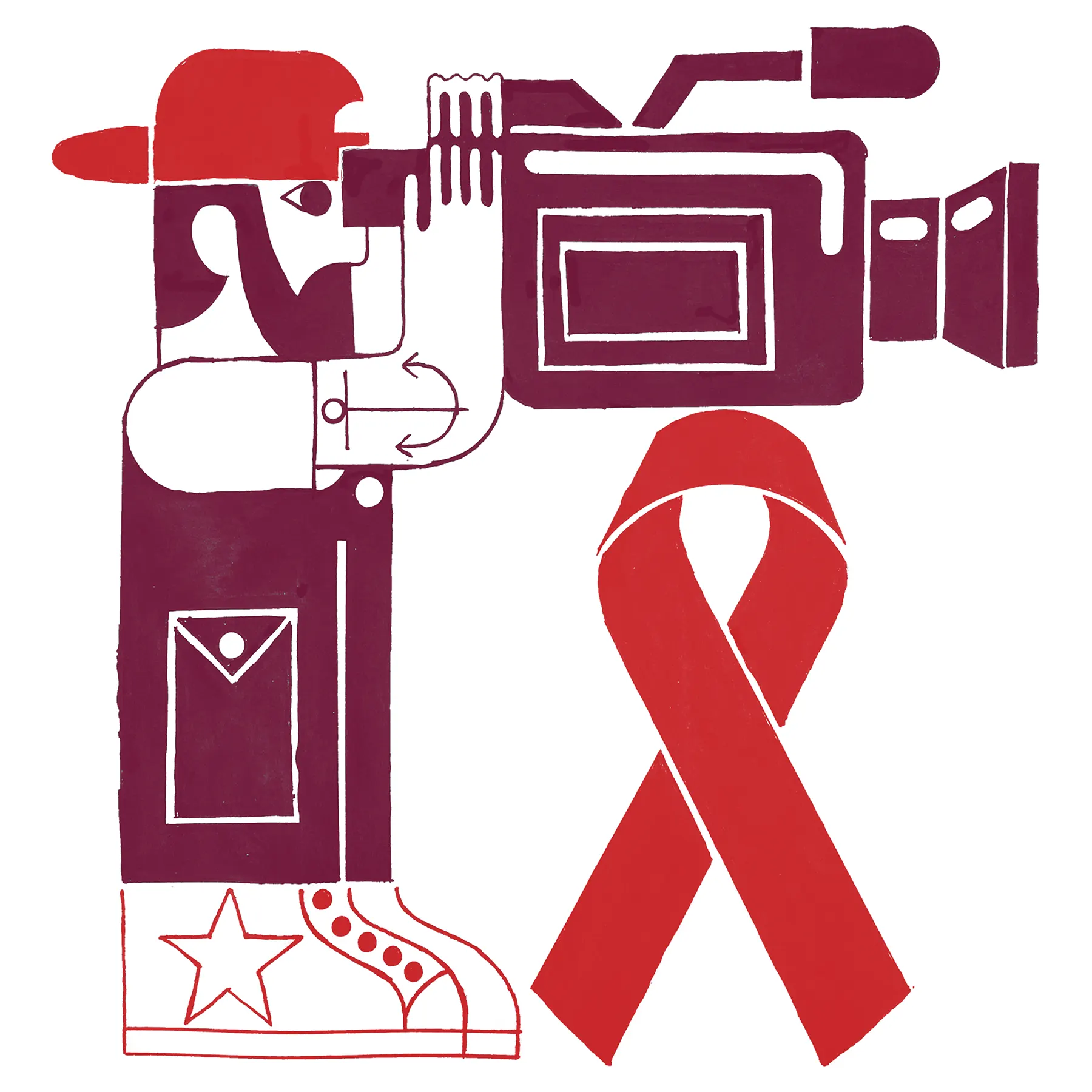
Videos will provide HIV education to young people
By Joey Garcia
Illustration by James Taylor
HIV prevention, care and education are crucial, but these programs typically target adults, leaving out another essential audience — adolescents. As clinical program manager of the Miller School’s Division of Adolescent Health, Alex Moreno, M.P.H., saw this demographic’s value. Within the division lies the Adolescent Counseling and Testing Service, geared to patients under age 29. At the clinic, managed by the Miami-Dade County Department of Health, Moreno and his staff see weekly STI cases in this age range, with the occasional instance of HIV infections occurring in young teenagers.
“Unfortunately, our school systems don’t offer the greatest education on sexual health,” Moreno said. “A perfect storm has risen in Miami-Dade County with adolescent HIV and STI infections due to issues with school funding, socioeconomic factors in the home and the lack of parental accountability.”
Current educational initiatives offer a typical textbook and outdated visual approach that has proven ineffective. Moreno knew a change had to be made and is working to create a series of videos with his nonprofit FLOW (Future Leaders of the World), a collaboration with the UM School of Communication’s Department of Cinematic Arts and with directorial support from renowned film director David Frankel.
Each of the seven videos will cover complex social topics such as HIV/AIDS and sex trafficking. They will be available in English and Spanish and will serve as a setup for an accompanying lesson plan. Moreno and his team are working to get the videos approved by the Florida School Board and become part of the health curriculum in Miami-Dade County, as well as in middle schools, high schools and colleges throughout the state.
“Our film premiere drew in 79 people with high ratings and support,” Moreno said. “These educational videos have the potential to make a dent in an often-overlooked demographic of Black and Latino adolescents in an impactful way.”
As HIV has no age limit, Moreno’s envisions expansion to those over 29. In collaboration with Positive People Network Inc., he plans to educate patients who are living with HIV through public advocacy, testimonial speeches and public service announcements showing that life doesn’t end with HIV.
Help on Wheels
The Mobile PrEP Program targets local HIV clusters
By Joey Garcia
Illustration by James Taylor
Extending out from the Miller School campus is the Mobile PrEP Program, which reaches into neighborhoods with HIV clusters including Miami Beach, Hialeah, Miami Gardens, Liberty City and South Dade. The initiative, which was launched in 2018 as a pop-up clinic offering PrEP (Pre-Exposure Prophylaxis) services in Miami Beach, is led by Susanne Doblecki-Lewis, M.D., M.S.P.H. ’17, professor of clinical medicine and chief of the Division of Infectious Diseases at the Miller School.
Dr. Doblecki-Lewis was involved in PrEP during its trial phase before it received FDA approval. During that time, she was an investigator on a demonstration project funded by the National Institutes of Health to see if people wanted to take the medication. The study showed people want access to PrEP, but after the study, in many places, Miami being one of them, lack of insurance, provider stigmas and bias, and time-off complications led to the lack of continuation.
“Our first mobile clinic was the result of various supporters, with the Florida Department of Health providing funding for a lab and staff, and Sylvester Comprehensive Cancer Center sharing their mobile Game Changer Vehicle with us,” Dr. Doblecki-Lewis said. “The power of mobile clinics lies in their ease of access outside of fixed locations and being more patient-centered.”
The Mobile PrEP program, which now has its own dedicated mobile clinic, rolls out five days a week and spends one day in each of the five local HIV clusters. It is open in the afternoon and evening, and always at the same spots to make the program more accessible. People requiring services can get free PrEP, PEP (to prevent HIV after a recent exposure within three days), STD and HIV testing, and rapid engagement in HIV care for those who test positive, along with educational information.
Such services are widely used predominantly by gay and bisexual Latino men, as well as by Black women. Around 900 HIV tests are performed yearly by the mobile clinic, and around 400 new PrEP prescriptions are dispensed. Those seeking more continuous care can access the fixed clinic run by Dr. Doblecki-Lewis on the medical campus. The program also offers free transportation services for those with HIV or on PrEP who seek care at the fixed clinic.
“In many ways we are a regular clinic, but with a more personal structure,” Dr. Doblecki-Lewis said. “Our program is developing trust with the community as we aim to close the HIV care gap in these areas of need.”
Eliminating HIV Through Prevention
 any people are hoping for an HIV vaccine but developing one may take several more years. In the interim, the U.S. has set a goal to reduce new HIV infections by 90% by 2030.
any people are hoping for an HIV vaccine but developing one may take several more years. In the interim, the U.S. has set a goal to reduce new HIV infections by 90% by 2030.
ART will play a key role in meeting those numbers, and long-lasting injectable drugs are making it easier for people to comply with their medication regimens. When patients’ HIV becomes undetectable, it reduces the chance of transmission to near zero. In addition, PrEP helps keep at-risk people safe from infection. Community outreach programs, like those at UM, will play a significant role in expanding PrEP’s use.
“HIV was a death sentence, and then we had treatments, but people had to take hundreds of pills. Now we can treat people with one pill,” Dr. Pahwa said. “And if we can get enough people the right medications, we can reach that 90% goal and really reduce the HIV burden in our community.”
Dr. Stevenson is similarly optimistic. “We don’t have a cure yet,” he said, “but we’re knocking on the door.”
If you’re interested in learning more or supporting our work, please contact Shelly Friedman, Senior Director of Development, at shelly.friedman@miami.edu.