Shedding Light on Hearing Loss
UM will test a new type of cochlear implant with exciting potential
By Josh Baxt
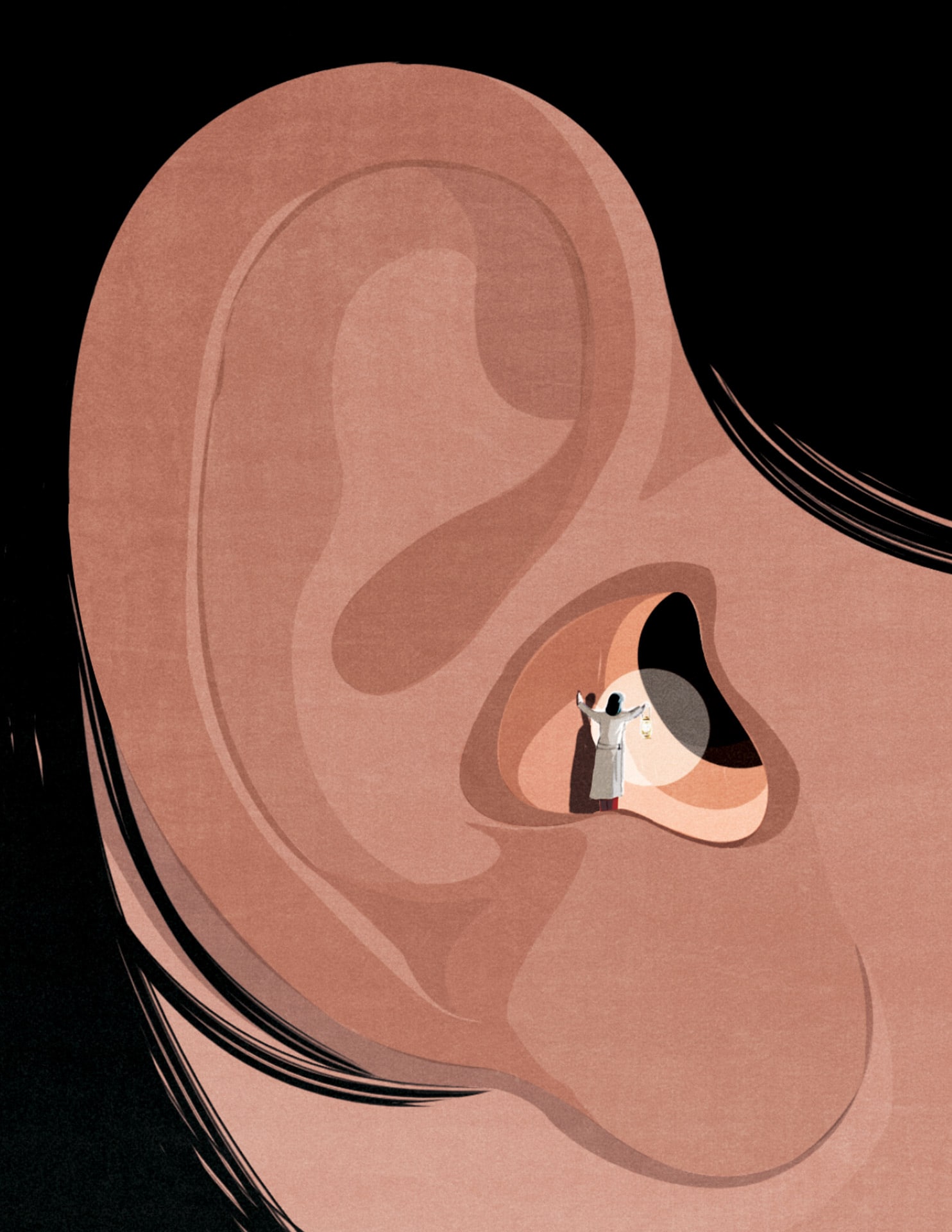
Illustration by Andrea Ucini
T
he University of Miami will be one of only three sites in the nation to test a potentially revolutionary opto-electrical cochlear implant, which could improve quality of life for millions of people with hearing loss.
The five-year study is funded by a major multi-institutional grant from the National Institute on Deafness and Other Communication Disorders. The team of UM investigators will be led by Suhrud Rajguru, Ph.D., associate professor of biomedical engineering and otolaryngology and co-director of the Institute for Neural Engineering; Jorge Bohorquez, Ph.D., associate professor of biomedical engineering; and Michael Hoffer, M.D., professor of otolaryngology.
Cochlear implants send electrical signals to the cochlear nerve to boost hearing. They are the world’s most successful neuroprosthetic to date, restoring partial function in nearly 700,000 people, including congenitally deaf children and adults, and those who lose their hearing from an infection or other causes.
Still, current implants utilizing electrical stimulation face limitations. Individual performance among recipients varies greatly; people with implants face difficulties enjoying music and often have trouble hearing conversation in loud rooms or against background noise.
“A normal cochlea transmits around 3,000 channels of information,” Dr. Rajguru said. “Current electrical implants replace that with somewhere between 16 and 22 channels only. It’s remarkable the brain makes sense of it at all.”
The implant being studied uses light in the infrared range to stimulate the cochlea and could potentially encode far more acoustic information.
“The advantage of light is that it can be focused and confined in space like a laser pointer,” Dr. Rajguru said. “We hope to generate 50 to 100 channels or possibly more to provide increased spectral selectivity for encoding sound. These devices could better replicate the cochlea’s natural ability to transmit signals to the brain.”
Trial participants will come from a small pool of people who have large tumors at the base of their skull, requiring translabyrinthine craniotomies to remove them — a procedure that damages the inner ear.
“We are not yet approved to permanently implant the device, and we have to proceed cautiously,” Dr. Rajguru said. “We hope that this study will allow us to go back to the FDA with the data and move forward with clinical translation.”![]()



