The Quiet Evolution

The Quiet Evolution
SHARE
Basic science research has three main goals: figure out the natural world, train the next generation of scientists, and generate discoveries that can become new diagnostics and therapies.
These are not separate goals but rather part of the same pipeline. Teams of researchers, including Ph.D. students, postdoctoral scientists, principal investigators and many others, work in concert to identify unique biological mechanisms. These findings are then published, sometimes sparking interest from biopharma companies.
Years later, the fruit of those initial inquiries may end up on pharmacy shelves. Still, that FDA-approved drug is just the tip of the iceberg; the fundamental discovery pipeline is the massive structure that most people never see. It’s a quiet evolution involving large-scale time and effort.
“As a clinician, I diagnose and treat patients with acute and chronic diseases, but it’s the basic scientists who help us understand the mechanisms behind those diseases,”said Maria Alcaide, M.D., Residency ’05, Fellowship ’07, professor of medicine and vice provost for research and scholarship. “How do people end up with those conditions? How do they originate at the molecular level, at the cellular level, and what can be done to accelerate diagnosis and treatment?”
This ecosystem has been a lifeline for patients. Anyone who has a relied on a statin to control their cholesterol or an immunotherapy to fight their cancer can attest to how important this pipeline can be. Virtually every drug developed over the past 50 years originated in an academic laboratory.
“Basic science is responsible for all the advances we have seen in modern medicine,” said Henri R. Ford, M.D., M.H.A., dean and chief academic officer of the Miller School. “By investing in basic science, we bring hope to humanity. Progress begins with us.”
Moreover, research offers a good return on investment. According to the National Institutes of Health (NIH), every dollar it spends on research produces an additional $2.50 in economic activity.
For decades, the Miller School has excelled at this work, expanding human knowledge, seeding new researchers around the world and providing the intellectual raw materials that advance medical care.
“Without that quest for knowledge about how a biological mechanism works and how it could be affected by disease, we wouldn’t be able to move forward with clinical applications,” said Norma Sue Kenyon, Ph.D., professor of surgery and executive director of the Wallace H. Coulter Center for Translational Research at the Miller School. “Without that fundamental knowledge, we would not have the continuum of translational and clinical research that leads to new therapies.”
“New knowledge has a ripple effect in the life sciences community.”
Norma Sue Kenyon, Ph.D.
The Pathway to Drug Development
Long before there’s an approved drug — or even before a molecule has been developed that could become a drug — researchers in the lab conduct in-depth investigations into how healthy cells function and why they sometimes become diseased.
During this painstaking process, scientists often create knockouts: organisms that are intentionally missing one or more genes. Through this subtraction process, investigators can determine what a gene does and what happens when it’s taken away.
In some cases, the knockout organism’s phenotype (its observable characteristics) can resemble the symptoms of a specific disease. This may not be a eureka moment, but it’s a powerful insight. If that knocked-out gene does indeed drive the disease, it could become a promising therapeutic target.
“It is essential that our research impacts human health,” said Stephen D. Nimer, M.D., director of Sylvester Comprehensive Cancer Center and executive dean for research. “The lab is a place for discoveries that could someday lead to a new understanding of a disease or even a new therapy. How exciting is it to do an experiment, and when you look at the result, you see a path forward to developing a novel drug?”
It would be hard to overstate how important this fundamental research process is to the drug discovery process. Developing a drug without knowing the target would be like trying to visit a friend without knowing their address or even the city where they live.
“We’re investing in fundamental research in neuroscience and aging because those are areas where we can truly be distinctive and impactful.”
Henri R. Ford, M.D., M.H.A.

Life sciences companies (and other researchers) are hungry for these discoveries, creating a symbiotic relationship. Biopharma scientists constantly scan the research literature, often using artificial intelligence, to find the scientific nuggets that could lead to new therapies. In some cases, they pay to license this intellectual property, providing additional resources for academic institutions, like the Miller School, to conduct more research.
“One of the principal ways industry discovers something unique is through publication,” Dr. Kenyon said. “When an investigator publishes a game-changing paper, industry is going to want to know more, and other universities are going to invite that researcher to conduct seminars. New knowledge has a ripple effect in the life sciences community.”
Sometimes that knowledge is expressed in a new database. Researchers at the John P. Hussman Institute for Human Genomics routinely share their genetic findings through open databases. This ongoing knowledge sharing helps keep the research moving forward, worldwide, and drives discovery.
Still, one of fundamental discovery’s most significant advantages is its flexibility. Studying a single biological mechanism could lead to insights into numerous diseases.
“I have the academic freedom to go where the science takes me,” said Claes Wahlestedt, M.D., Ph.D., professor, director of the Center for Therapeutic Innovation and associate dean for therapeutic innovation. “If I’m working on a neuroscience project but find a target that might be useful in oncology, I can apply for a grant and pursue it. That would be harder in industry, which is more narrowly focused.”
The Drug Discovery Timeline
10 steps from the laboratory bench to the pharmacy shelf
1
2
3
4
5
6
7
8
9
10
Growing Scientific Talent
There’s a persistent myth that science is advanced by gifted loners who toil away in isolation. In reality, science is a team sport. Principal investigators (PIs) like Dr. Wahlestedt are basically lab CEOs, providing scientific and logistical direction for their research teams. Most of the day-to-day scientific work is conducted by Ph.D. students and postdoctoral researchers. Such PIs are typically also open to collaborations anywhere to fill project gaps.
Postdoctoral positions are much like scientific apprenticeships, during which young researchers hone their lab skills. This goes well beyond benchwork. “Postdoctoral training is where people absorb how labs operate and what it would be like to run their own lab,” said Joan St. Onge, M.D., M.P.H. ’18, professor of clinical medicine and senior associate dean for faculty affairs and professional development.
In this latter role, Dr. St. Onge and colleagues help junior faculty, often recently promoted postdocs, advance their research and careers.
“Researchers get so focused on the science, they can neglect some of the finer points of career advancement,” she said. “They may need help being a good mentor, as well as a good mentee, for example. These processes are essential to support effective science.”
Sometimes, researchers come from the clinical side. Physician scientists often see problems they are uniquely qualified to address and are driven to solve them. Alessia Fornoni, M.D., Ph.D., Fellowship ’01, co-directs the Medical Scientist Training Program (MSTP), which helps physician trainees combine medicine and research.
She also co-directs the Clinical and Translational Science Institute’s Mentored Translational Research Scholars Program, which helps gifted young scientists advance their science. These groups closely collaborate to provide a web of support for physicians and bench researchers to help boost discovery.
The University of Miami is deeply committed to supporting scientists and accelerating their work. In 2024, the university committed $30 million over five years to give researchers the necessary resources to better understand biology and develop new clinical interventions. The funding will specifically support investigations into neuroscience and aging.
“We’re investing in fundamental research in neuroscience and aging because those are areas where we can truly be distinctive and impactful,” Dean Ford said.
“We are committed to sustaining a culture that creates and supports physicians and scientists in all disciplines and enhances the basic sciences,” Dr. Alcaide said. “Our robust research environment is built on people in our labs and our clinics who are smart, innovative and creative, and are outstanding clinician and scientists. We want to provide them with the necessary resources to ensure their success in advancing health sciences.”
“I have the academic freedom to go where the science takes me.”
Claes Wahlestedt, M.D., Ph.D.
Asking Questions, Finding Answers
All these endeavors — the research, the education, the supportive environment — combine to help scientist develop new ideas and carry them forward. But dig down to the roots and the defining element is pure human curiosity. Researchers and clinicians have questions, and they are driven to find the answers.
Dr. Fornoni is just one of many examples of such researchers. In addition to her administrative roles, she is a Miller School-trained nephrologist and has witnessed first-hand the gaps in kidney care.
“I am always frustrated to shake hands with some of my patients at the end of the visit and say: ‘I’m sorry, there’s not much else we can do,’” she said. “So, I closed the loop. I observed my patients, I brought those insights to the bench, and I discovered two drugs.”
Her research focuses on how lipids (fat) contribute to kidney fibrosis, ultimately forcing her patients to seek dialysis or transplant surgery.
Both of her drugs are designed to reduce the lipids that get trapped in the parenchyma — the kidney tissue in charge of filtering the blood. One of these drugs, a sugar molecule called VAR 200, has been licensed by ZyVersa Therapeutics, a company Dr. Fornoni founded along with several other Miller School faculty in 2014.
Both drugs have been found safe in early trials and have great potential to slow kidney disease, particularly a rare genetic condition called Alport syndrome.
“It’s incredibly rewarding to be a physician scientist because, when you look at a disease, you don’t have to just follow the approaches developed by others — you are the one developing new approaches through your science,” Dr. Fornoni said. “It becomes like an addiction to be a physician-scientist, a very good one to have.”
“How exciting is it to do an experiment, and when you look at the result, you see a path forward to developing a novel drug?”
Stephen D. Nimer, M.D.
A Hunger for Discovery
This hunger to discover permeates the Miller School, and is generally only slowed by global catastrophes, like the COVID-19 pandemic, and disjointed funding. Several research projects have become approved treatments. Others, like Dr. Fornoni’s kidney drugs, are winding their way through human clinical trials.
Camillo Ricordi, M.D., professor of surgery and medicine and chief of the Division of Cellular Transplantation at the Miller School’s Diabetes Research Institute, and Dr. Kenyon have spent three decades working on a drug that can dampen the immune response to transplanted pancreatic islet cells — a critical technology that has the potential to cure type 1 diabetes. Their patience and persistence paid off with the drug tegoprubart, which is currently in clinical trials to modulate immunity, as well as being tested as a treatment for amyotrophic lateral sclerosis, or ALS.
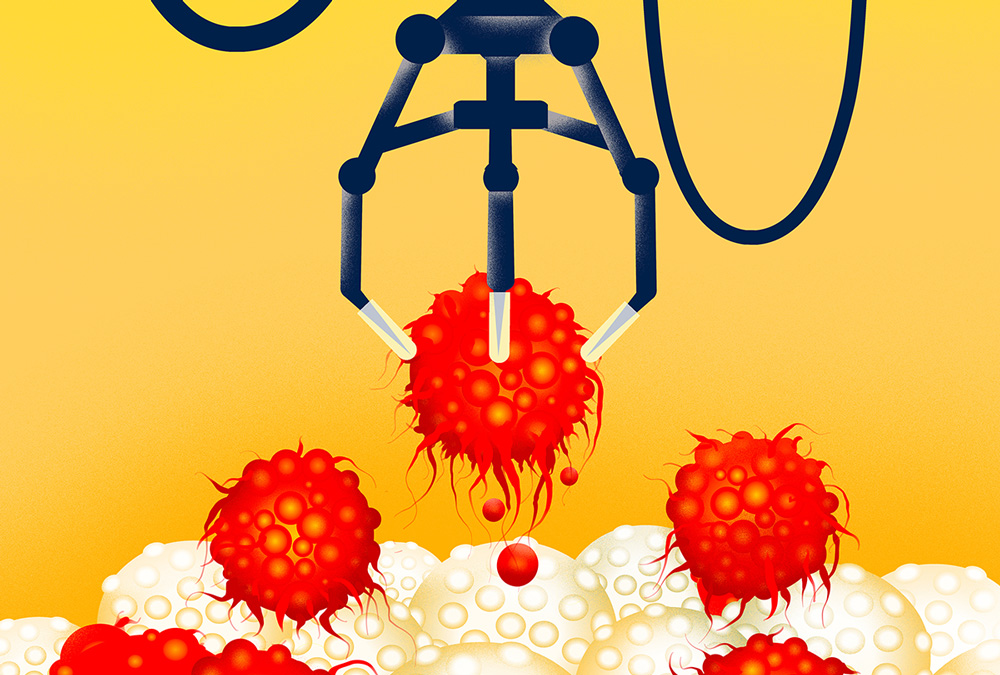
Dr. Wahlestedt helped discover a drug, EP31670 that reprograms cancer cells to make them easier to kill. The drug targets the epigenome, which reacts to environmental cues to manage how certain genes are expressed. Unfortunately, the epigenome can go awry in cancer and be co-opted to support tumor growth. Taking control of these mechanisms could help move the needle on cancer care. EP31670 is now undergoing clinical trials for blood cancers at the University of Miami and several other trial sites. Dr. Wahlestedt also continues his longstanding efforts on RNA-targeted drugs.
Thomas Malek, Ph.D., professor and chair of the Department of Microbiology and Immunology, has spent many years trying to understand how immune cells are regulated. Those efforts have translated into a new drug, called IL2-CD25, which has great potential and is under commercial development for autoimmune diseases.
IL2-CD25 modulates immunity by providing consistent, low-dose interleukin 2 (IL2) to dampen the autoimmune response. This solves a thorny problem that has plagued the medical community for decades: instead of broadly suppressing the immune system to reduce autoimmunity, IL2-CD25 resets the immune system in a way to restore immune processes that normally function to prevent an autoimmune attack from starting in the first place. Dr. Malek’s approach is currently in a phase 1B clinical trials for lupus, an autoimmune condition that can cause chronic inflammation in multiple organs and atopic dermatitis, a chronic inflammatory skin condition.
These scientists, and hundreds of others at the Miller School, channel their curiosity, intuition and drive to contribute new knowledge and, in some cases, new medicines. Their efforts are the roots that feed all patient care.
“It’s not just basic sciences research, it’s surgical research, it’s devices, it is really everything that you can picture to enhance clinical activities in clinical settings and promote health,” Dr. Alcaide said. “The tools of our diagnostic processes — the laboratory tests used to diagnose and prevent diseases by examining our blood, the imaging machines that allow us to diagnose without invasive procedures — and the development of new pharmacological treatment and devices all have their origin in research laboratories. Every scientist on Earth, whether they are at a university or in industry, learned the basics of their professions in academic laboratories. It’s a process that saves lives every day, and we must continue to support it.”
“It’s a process that saves lives every day, and we must continue to support it.”
Maria Alcaide, M.D.
Invented Here
AI-Powered Vision Care

Improving Cancer Treatment
Easier Access for Neurosurgery
Eric Cecala Peterson, M.D., Fellowship ’13, professor of clinical neurosurgery and neuroradiology, founded RIST Neurovascular, which developed the RIST catheter. Prior to that, neuroradiologists had to insert catheters in the femoral artery in the thigh, which made these procedures quite challenging. Instead, they can insert the RIST catheter through the radial artery in the wrist, which provides a much simpler path to the brain. Medtronic now owns the technology.

A Tool for Better Eye Surgery
21st Century Pathology
Azorides Morales, M.D., who chaired the Miller School’s Department of Pathology and Laboratory Medicine for 33 years, and colleagues, wondered if there was a way to process patient biopsy samples faster. Their solution was a rapid tissue processor, which accelerated processing times from days to hours. As a result, patients and clinicians can move rapidly into diagnosis and treatment. The instrument was licensed to Sakura.

A Unique Approach to Mental Health Care
Jose Szapocznik, B.S. ’69, Ph.D. ’77, professor of public health sciences and director of the Center for Family Studies, and Miller School clinical psychologist Joan Muir, Ph.D., developed a software platform that provides brief strategic family therapy. The technology is being deployed by Empower, an evidence-based mental health care provider.